Healthcare interoperability is the foundation for effective data exchange and communication across today’s complex health systems.
As healthcare organizations manage increasing volumes of electronic health records and patient data, the ability to share accurate health information securely and efficiently is essential for delivering high-quality patient care and meeting regulatory requirements.
Today, we’ll review the importance of healthcare interoperability, including four key types that provide healthcare organizations with better visibility and comprehension of their document management processes.
Key Takeaways
- Use the four HIMSS-defined levels—foundational, structural, semantic, and organizational—to evaluate your current interoperability capabilities, identify specific gaps, and create a targeted plan for improvement.
- Implement widely recognized standards such as HL7, FHIR, and SNOMED CT to ensure your systems can securely and accurately exchange, interpret, and use electronic health information across multiple platforms and organizations.
- Upgrade EHR and document management systems to support structured and standardized data formats, and provide ongoing training to staff on using these systems and following best practices for data sharing.
- Tackle challenges like fragmented systems, lack of standardization, and resource constraints by developing strong data governance policies, investing in secure infrastructure, and fostering collaboration across departments and partner organizations.
- Collaborate with experienced document management service providers to implement scalable content management systems that support seamless, compliant, and interoperable exchange of patient information—improving care coordination and operational efficiency.
What Is Healthcare Interoperability?
Healthcare interoperability is the ability of different health information technology systems, devices, and software applications to seamlessly exchange, interpret, and use health data—regardless of the organization, location, or technology involved.
This means that electronic health records, clinical data, and patient information can move securely and efficiently between healthcare providers, payers, and patients, supporting coordinated care and better health outcomes.
In practice, interoperability enables health systems to share accurate patient data in real-time, providing providers with the necessary information to deliver safe and effective care.
Achieving interoperability relies on the adoption of data exchange standards, such as Fast Healthcare Interoperability Resources (FHIR), and the use of secure, interoperable systems that protect patient privacy while enabling timely access to critical health information.
The Four Levels of Healthcare Interoperability
The Healthcare Information and Management Systems Society (HIMSS) defines four distinct levels of healthcare interoperability: foundational, structural, semantic, and organizational.
Each level builds on the previous, guiding healthcare organizations toward more effective, accurate, and seamless data exchange.
Understanding and advancing through these levels is essential for health systems aiming to optimize patient care, reduce inefficiencies, and achieve regulatory compliance.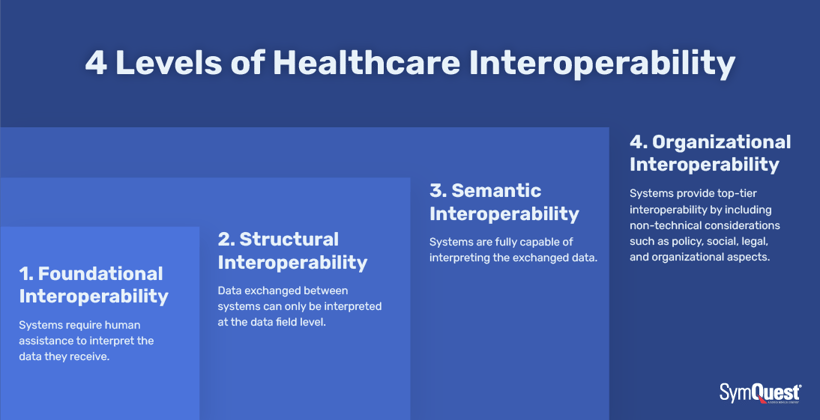
1. Foundational Interoperability
Foundational interoperability is the most basic level, enabling one health information system to send and receive data from another. At this stage, systems can exchange data, but the receiving system may not be able to interpret or use the information without human intervention.
This level focuses on establishing secure connectivity and basic data transport between disparate systems, such as EHR platforms, document management systems, or medical devices. The primary goal is to ensure that data can move from point A to point B, even if it cannot be automatically processed or understood by the receiving system.
Take this example: a hospital’s EHR exports a patient’s discharge summary as a PDF and transmits it via secure email to a primary care provider. The provider receives the document but must review and manually enter relevant details into their own system.
Foundational interoperability is critical for breaking down initial barriers to data exchange. It enables basic communication between healthcare entities, which is essential for timely information sharing, especially in urgent care scenarios.
Without foundational interoperability, health data remains siloed, leading to delays in care, redundant testing, and increased administrative burden. Providers may have to rely on phone calls, faxes, or paper records, increasing the risk of errors and inefficiencies.
To achieve it:
- Implement secure data transfer protocols (e.g., Direct secure messaging, VPNs).
- Use interface engines or health information service providers (HISPs) to facilitate basic data exchange.
- Ensure systems can at least send and receive standard file formats (e.g., PDFs, HL7 messages)
2. Structural Interoperability
Structural interoperability standardizes the format, syntax, and organization of exchanged data so that receiving systems can correctly parse and display the information.
At this level, data fields are organized according to agreed-upon standards (such as HL7 or Fast Healthcare Interoperability Resources [FHIR]), allowing systems to automatically identify and process specific pieces of information—like patient demographics, lab results, or medication lists—without manual intervention.
Here’s how it could work.
A primary care provider refers a patient to a specialist using a standardized electronic referral form. The specialist’s EHR system automatically imports the patient’s information, diagnosis, and reason for referral, preserving the structure and intent of the data.
Structural interoperability reduces manual data entry, minimizes errors, and ensures that critical information is not lost or misinterpreted during transfer. It supports more efficient workflows and better care coordination.
Without structural interoperability, even if data is exchanged, it may arrive in unstructured formats (like free-text notes or scanned documents), requiring time-consuming manual processing and increasing the risk of miscommunication.
For this you’ll need to:
- Adopt industry data standards such as HL7, FHIR, or CDA.
- Upgrade EHR and document management systems to support structured data exchange.
- Train staff on using standardized forms and templates for data entry and sharing
3. Semantic Interoperability
Semantic interoperability ensures that exchanged data is not only structured but also interpreted and used consistently across systems, preserving its clinical meaning.
This level relies on standardized vocabularies and coding systems (e.g., SNOMED CT, LOINC, ICD-10) so that information like diagnoses, lab results, and procedures are understood the same way by all systems and providers.
Semantic interoperability enables true machine-to-machine communication, supporting advanced analytics and clinical decision support.
Here’s what this looks like.
A patient’s allergy information, coded using standard terminology, is shared between hospital and pharmacy systems. Both systems recognize the allergy, preventing the prescription of contraindicated medications.
Semantic interoperability is crucial for accurate clinical decision-making, population health management, and reducing medical errors. It allows health systems to aggregate and analyze data for research, public health, and quality improvement initiatives.
Without semantic interoperability, data may be misinterpreted or rendered meaningless, leading to errors in diagnosis, treatment, and reporting. Ambiguity in data can result in patient harm and increased healthcare costs.
To get this, you’ll:
- Implement and map to standardized clinical terminologies (SNOMED CT, LOINC, ICD-10).
- Use middleware or integration platforms to translate and normalize data between systems.
- Engage clinical informatics experts to oversee data standardization and mapping
4. Organizational Interoperability
Organizational interoperability is the highest level, encompassing the governance, policies, legal frameworks, and workflows needed for seamless data sharing and use across different organizations and systems.
This level addresses not just technical integration, but also the alignment of business processes, trust frameworks, and data governance.
It ensures that healthcare organizations—such as hospitals, clinics, insurers, and public health agencies—can securely and efficiently collaborate, share, and act on health information in compliance with legal and ethical standards.
Organizational interoperability enables large-scale care coordination, population health management, and public health reporting. It is essential for initiatives like Accountable Care Organizations (ACOs), integrated delivery networks, and disaster response.
Without organizational interoperability, even technically compatible systems may not be able to share data due to policy, legal, or workflow barriers. This leads to fragmented care, inefficiencies, and missed opportunities for improving patient and population health.
Here’s how you can achieve it:
- Develop and enforce data governance policies and trust frameworks.
- Participate in regional or national HIEs and adopt frameworks like the Trusted Exchange Framework and Common Agreement (TEFCA).
- Align organizational processes and workflows to support secure, compliant data sharing across entities.
Evaluating your organization’s current interoperability level and identifying gaps is the first step toward building a more connected, efficient, and patient-centered healthcare system.
Each advancement—from foundational to organizational interoperability—delivers greater value, supporting better patient outcomes, reduced errors, and more effective care delivery.
Why Healthcare Interoperability Matters for Health Systems and Patient Care
Modern healthcare relies on a network of interconnected providers, health information systems, and medical devices. Without seamless interoperability, critical patient health information can become trapped in isolated systems, leading to incomplete records, communication gaps, and missed opportunities for care coordination.
Interoperable health information exchange enables:
- Comprehensive Patient Records: Consolidating clinical data from multiple systems provides a longitudinal patient record, giving healthcare professionals a complete view of a patient’s health history.
- Improved Patient Safety: Access to accurate data reduces medical errors and helps prevent patient harm by ensuring providers have the information needed for informed decision-making.
- Enhanced Care Coordination: Timely and seamless portability of health data supports collaboration among healthcare providers, improving patient outcomes and streamlining transitions of care.
- Regulatory Compliance: Meeting standards set by organizations like the National Coordinator for Health Information Technology and adhering to frameworks such as Fast Healthcare Interoperability Resources (FHIR) and United States Core Data for Interoperability (USCDI) helps health systems align with federal and industry requirements.
- Operational Efficiency: Automated, interoperable systems reduce administrative burden, improve data quality, and enable healthcare organizations to focus resources on patient care.
As the healthcare industry continues to evolve, promoting interoperability is critical for supporting secure data exchange, protecting patient health information, and driving better health outcomes across the healthcare enterprise.
Barriers to Healthcare Interoperability
Despite the clear benefits of seamless health data exchange, healthcare organizations continue to face significant obstacles on the path to true interoperability.
These barriers stem from both technical and organizational challenges that impact the quality, accessibility, and security of electronic health information across health systems.
Here are some of the biggest obstacles:
Fragmented and Siloed Systems
Many healthcare organizations operate with a patchwork of electronic health record (EHR) systems, medical devices, and health information exchanges that use incompatible data standards. This fragmentation leads to data silos, making it difficult to share patient health information efficiently and accurately.
Legacy Technology and Technical Debt
Outdated legacy systems often lack the capacity to integrate with modern health information technology or support secure data exchange. Maintaining these older interfaces increases operational costs and creates bottlenecks in the flow of electronic health data.
Lack of Standardization
The healthcare industry relies on a wide variety of data exchange standards (such as HL7, FHIR, and proprietary formats). Inconsistent adoption of these standards results in challenges with data mapping, patient matching, and the usability of exchanged information.
Resource Constraints
Implementing interoperable systems requires significant financial investment and skilled personnel. Many organizations, especially smaller clinics or rural health departments, struggle to allocate the necessary resources for upgrading systems and training staff.
Security and Compliance Concerns
As the volume and sensitivity of patient data grows, so does the risk of data breaches and cyber threats. Ensuring secure data exchange and compliance with regulations like HIPAA adds complexity to interoperability initiatives.
Organizational Resistance and Data Ownership
Beyond technical hurdles, organizational structures and concerns about data ownership can slow progress. Competing priorities, reluctance to share data, and information blocking by some stakeholders further impede the creation of interoperable health information networks.
Operational Inefficiencies
Manual processes, such as faxing or mailing patient records, persist in many settings, undermining the potential of electronic health information to improve care coordination and patient outcomes.
The consequences of these barriers are far-reaching. Fragmented patient records can delay critical care decisions, increase administrative burden, and contribute to provider burnout.
During public health emergencies, such as the COVID-19 pandemic, limited access to external patient data has directly impacted the ability of hospitals to deliver timely, effective care.
Overcoming these challenges requires a coordinated effort to modernize health information systems, adopt common data standards, invest in secure infrastructure, and foster a culture of collaboration across the healthcare industry.
Advance Your Healthcare Organization’s Interoperability Initiatives with Document Management Services
To improve patient care and operational efficiency, healthcare providers should make interoperability a strategic priority.
Partnering with an experienced document management service provider can help healthcare organizations implement an intuitive, scalable content management system that securely stores and shares medical information.
This approach enables the seamless, interoperable exchange of patient data—supporting better care coordination, reducing administrative burden, and ensuring compliance with evolving health information standards.





